-
9th April 2019, 10:30 AM
#1
Iridium

Candida auris, a superbug fungal strain Infects hospitals worldwide
Link
(Natural News) Imagine a dystopian science-fiction future where hospital ventilation systems are pumping out a deadly superbug, right into the open atmosphere, where winds carry it to local communities and farms, infecting crops and foods with chemical-resistant fungal strains that have a reported 41% – 88% fatality rate in humans. And imagine the CDC knew about it, but refused to tell you which hospitals were infected. Local hospitals hid the fact that their own hospital rooms and intensive care units were being overrun with this fatal fungi, and that all the world’s epidemiological experts had no idea where the pathogen had come from or how to stop it.
But they all kept it a secret, because they didn’t want to “alarm” the public. And they sure didn’t want hospitals to be seen as hubs of superbug infections.
Well, imagine no more. This is real. It’s happening right now. And this pandemic has been silently spreading over the last four years, with virtually zero media reports, very little information from the CDC, and a coordinated cover-up by the hospitals of the western world to keep patients in the dark while they’re being infected and killed by a deadly pathogen.
This is the true story of Candida auris, a superbug fungal strain that has emerged from the widespread use of chemical fungicides in agriculture. In this extended Natural News report — initially based on a New York Times report but significantly expanded — you will learn why this silent pandemic has already invaded America’s hospitals and why it cannot be stopped using any known medical defense. It may already be too late for the planet. By abusing agricultural chemicals, humanity has given rise to a superbug that could, under the right conditions, kill a billion people and collapse the entire western medical system.
The power of the elements: Discover Colloidal Silver Mouthwash with quality, natural ingredients like Sangre de Drago sap, black walnut hulls, menthol crystals and more. Zero artificial sweeteners, colors or alcohol. Learn more at the Health Ranger Storeand help support this news site.
And you may already be “colonized” by this fungus, serving as a carrier who will infect others in your own family and community.
How did this happen? Understanding Candida auris
According to a bombshell New York Times investigation — yes, even the New York Times occasionally commits acts of real journalism — this pandemic has already found its way into some of the largest hospitals in New York, Chicago and London. The superbug fungus has spread to nursing homes and is carried from patient to patient by health care workers. It grows on IV lines and ventilators, and it infects hospital gowns and clothing. Aggressive sterilization efforts using aerosolized hydrogen peroxide do nothing to kill this fungus, and the cover-up continues, even as rates of infections and fatalities are exploding across the western world.
The fungus is called Candida auris, or C. auris for short. It’s called Auris because it was originally discovered to be living in a woman’s ear in Japan. But now, it has spread to every continent, and its rise has only been made worse by a coordinated cover-up by the CDC, hospitals and the corrupt medical industry that places its own profits over the safety of the public. If there were a vaccine for Candida auris, these infections would be front page news across the globe, and journalists would be screaming at everyone to get injected with the vaccine. But since the medical establishment has no treatment whatsoever for this deadly pathogen, they’ve conspired to cover it up.
This Natural News report aims to explain how this happening and how the science lies of the chemical agricultural giants have now put the entire human race at risk from this exploding superbug pathogen.
To understand how we got here, we have to go back a few years and take a closer look at fungi that grow naturally in crop soils.
The mass chemical contamination of farm soils in the name of “crop yields”
Soil is a complex living ecosystem, and soils naturally harbor an astonishing array of microbiology, including bacteria, fungi and viruses. In healthy soils, the most dangerous organisms are crowded out by good organisms. This survival competition keeps the really nasty bugs in check, preventing them from expanding their colonies and gaining ground.
But modern farming relies heavily on chemical pesticides, herbicides and fungicides. These chemicals, which are routinely sprayed on food crops, demonstrate selective chemical toxicity that kills some organisms but leaves others untouched. Even worse, some strains develop resistance to agricultural chemicals through a process of adaptation and microbiological natural selection. This leads to the rise of so-called superbugs. (See Superbugs.news for more reports.)
“Superbugs” is a generic term that can apply to insects that develop chemical resistance, or it can describe microbes and even fungi that develop resistance to chemicals that would otherwise kill them. Any organism that survives the onslaught of toxic chemicals and develops a physiological survival mechanism to nullify or eliminate those chemicals will suddenly find itself able to grow and spread at a ferocious rate. That’s because its competition has been wiped out by the agricultural poisons such as fungicides. So as farmers sprayed fungicides on virtually every vegetable and fruit crop in existence, this practice led to the inevitable rise of a superstrain of Candida auris, which now finds itself able to replicate and spread in ways that never could have been possible when all the other fungi were competing for the same resources.
Killing off the “good” fungi, in other words, allowed the really dangerous fungal strains to succeed like never before. And the more chemicals are sprayed on food crops, the more dangerous the pathogens become. This is all caused by human intervention via chemical agriculture — an artificial way to produce food for the masses.
Millions of tons of fungicides are sprayed on food crops every year in the United States alone
By 2023, it is estimated that annual expenditures on fungicides will reach $21 billion worldwide. In 2016, an average of 4.26 pounds of fungicide chemicals were applied per acre in the United States, and one of the largest classes of fungicide chemicals is called “azole fungicides.”
Azole fungicides now account for one third of global sales of fungicides, and various derivatives of azoles are heavily applied to crops every day, all over the world, including triazoles and benzimidazoles. These chemicals end up not merely in our food, but in agricultural runoff, eventually contaminating water supplies, rivers and even oceans. Over time, as these azole chemicals were repeatedly applied to food crops year after year, Candida auris developed robust immunity to these chemicals, enabling the fungus to survive on food crops due to the fact that it now had no competition, since most other fungi strains were killed by the chemicals.
So crops harvested from food fields carried this fungus to food markets and grocery stores. There, consumers purchased the products and prepared them at home, touching those fruits and vegetables with their bare hands and transferring the fungal colonies to their homes, their clothing and other family members. Almost instantly, Candida aurisspread from foods to home environments, persisting in damp kitchens, dark drawers and closets, effectively colonizing humans who then carried it to other humans.
From here, it was only a matter of time before C. auris found its way to hospitals, nursing homes, surgical centers and retirement centers. Today, C. auris is no doubt colonizing children in day care centers; co-workers in office environments; friends at social gatherings and family members at holiday events.
Everything in hospital rooms is infected: The bed rails, window shades, curtains, doors, bed and even the ceiling
When a man died at Mount Sinai hospital in Brooklyn after being infected with C. auris, his hospital room was tested for the pathogen, reports the New York Times:
“Everything was positive — the walls, the bed, the doors, the curtains, the phones, the sink, the whiteboard, the poles, the pump,” said Dr. Scott Lorin, the hospital’s president. “The mattress, the bed rails, the canister holes, the window shades, the ceiling, everything in the room was positive.”
The fungus preys on those with weakened immune systems, including infants and the elderly. Its symptoms include extreme fatigue, and in certain immune-weakened populations, it has so far been observed to kill 41% of those it infects. (See below for more statistics showing an even higher fatality rate.)
People with strong immune systems are apparently able to fight off the effects of the fungus, but even if they show no symptoms, they may be carriers of the strain, infecting others who may suffer from weakened immune function. This includes infants and seniors, but can also impact those who have caught a cold or a flu, or even people who have endured an extremely strenuous workout at the gym, placing themselves in an immunosuppressed condition for 2-3 days. “[T]hey are most lethal to people with immature or compromised immune systems, including newborns and the elderly, smokers, diabetics and people with autoimmune disorders who take steroids that suppress the body’s defenses,” the NYT explains.
It is self-evidence that C. auris will also attack those who are taking antibiotics, as their own personal gut flora are wiped out by the antibiotic drugs in exactly the same way that friendly fungi are wiped out across crop fields by azole fungicide chemicals. Thus, the people who undergo surgical procedures at hospitals and are routinely given antibiotics as part of the treatment are also being kept in the very same hospital rooms where Candida auris is increasingly festering.
This combination is a public health catastrophe waiting to happen. Hospitals have now become colonization centers where humans are exposed to deadly fungi. Hospitals, in a very real sense, are spreading the pandemic. Again, from the NYT:
[T]he germs are easily spread — carried on hands and equipment inside hospitals; ferried on meat and manure-fertilized vegetables from farms; transported across borders by travelers and on exports and imports; and transferred by patients from nursing home to hospital and back.
Five warnings from the CDC’s fungal expert, Dr. Tom Chiller
The CDC’s own chief of its fungal research division, Dr. Tom Chiller, warns about Candida auris, “behaving in unexpected and concerning ways, causing severe disease in countries across the globe, including the United States.” In a Medscape article published in 2017, Dr. Chiller lays out some facts about Candida auris that even the New York Times decided not to report. Via Dr. Chiller’s warning: (my comments are added in parenthesis)
Warning #1) C auris can spread between patients in healthcare facilities and cause outbreaks. In this way, it appears to behave much like some multidrug-resistant bacteria (eg, methicillin-resistant Staphylococcus aureus or Acinetobacter).
Warning #2) C auris can colonize a patient’s skin for months or longer. (Yes, months. That means carriers can remain carriers for a very long time.)
Warning #3) This hardy yeast can live on surfaces for a month or more, and preliminary testing suggests that quaternary ammonium compounds commonly used for healthcare disinfection may not be sufficiently effective against C auris. (In other words, the usual chemicals that hospitals use to clean rooms simply don’t work against Candida auris.)
Warning #4) C auris is quickly becoming more common. In some international healthcare facilities, it has gone from an unknown pathogen to a cause of 40% of invasive Candida infections within a few years. We need to act now to prevent this from happening in the United States. (Too late. It’s also endemic in U.S. hospitals in Illinois, New Jersey and New York, although the CDC refuses to tell us which hospitals have been colonized by the fungus.)
Warning #5) C auris is often multidrug resistant. Some strains have been resistant to all three major antifungal classes, including echinocandins, the first-line treatment for Candida infections.
But it’s far worse than all that, in reality. Candida auris is airborne, and it floats through the air inside hospitals, infecting patients, hospital staff and colonizing hospital rooms and surgical areas. Even worse, the deadly pathogen is now escaping hospitals and infecting surrounding communities. Hospitals have, in effect, become hubs for spreading this deadly superbug across the country and around the world.
“Aerial samples of hospitals” test positive for the deadly pathogen… hospitals are factories that churn out this deadly disease
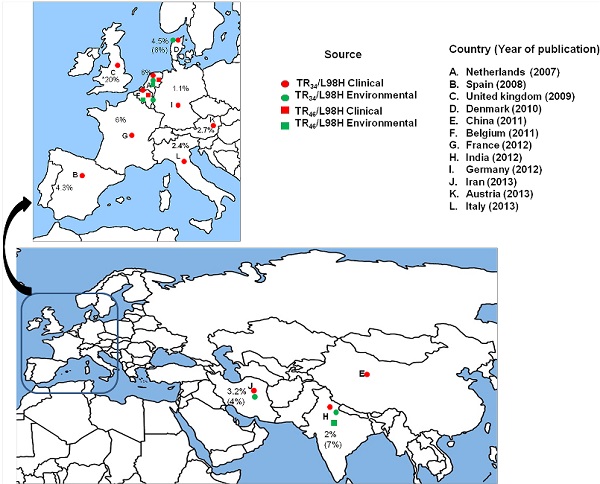
In 2013, a published science paper examined the spread of azole-resistant Aspergillus fumigatus arising from the agricultural use of azole fungicides. The paper was published in PLOS Pathogens with the title, “Emergence of Azole-Resistant Aspergillus fumigatus Strains due to Agricultural Azole Use Creates an Increasing Threat to Human Health.”
The paper supports the astonishing conclusion that people are acquiring fungicide-resistant strains through “environmental sources” rather than experiencing fungal mutations in their own bodies while being treated with anti-fungal drugs. As the study explains:
Several recent findings support the hypothesis that ARAF (azole-resistant A. fumigatus) strains in patients with invasive aspergillosis were more likely to be acquired from environmental sources rather than from de novo mutation and selection within patients during azole therapy.
The supporting evidence for this extremely disturbing realization is also cited by the science paper as follows:
#1) “ARAF strains have been found in patients who had never been treated with azole antifungal drugs.”
#2) “ARAF strains have been found in many environmental niches including flowerbeds, compost, leaves, plant seeds, soil samples of tea gardens, paddy fields, hospital surroundings, and aerial samples of hospitals.” This means that hospitals are effectively pumping out the fungal strains to surrounding areas.
#3) “These strains showed cross-resistance to voriconazole, posaconazole, itraconazole, and to six triazole fungicides used extensively in agriculture.” In other words, the fungus is almost certain to have emerged from repeated exposure to agricultural fungicides, since those are the chemicals for which it has developed innate resistance.
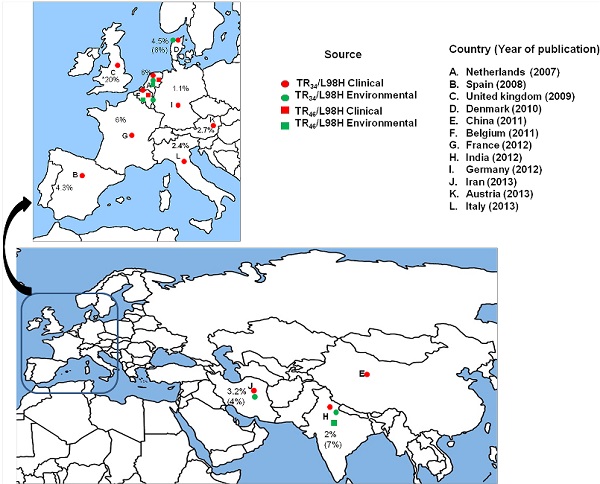
As the paper explains, it is the agricultural use of azole fungicides that supplies the most likely explanation for fungicide-resistant superbug fungi:
For example, azole fungicides are broadly used to control mildews and rusts of grains, fruits, vegetables, and ornamentals; powdery mildew in cereals, berry fruits, vines, and tomatoes; and several other plant pathogenic fungi. Over one-third of total fungicide sales are azoles (mostly triazoles) and over 99% of the DMIs (demethylase inhibitors) are used in agriculture. In addition, there are over 25 types of azole DMIs for agricultural uses, far more than the three licensed medical triazoles for the treatment of aspergillosis. Furthermore, the azoles could persist and remain active in many ecological niches such as agricultural soil and aquatic environments for several months.
The widespread application of fungicide for agricultural use, in other words, is the credible, rational explanation for the widespread development of azole-resistant fungi strains that colonize and kill people, including people who have never been known to carry the non-resistant strains in the first place.
Azole-resistant Aspergillosis killed human patients with a mortality rate of 88%
One of the most horrifying findings of scientists who study azole-resistant fungi is the startlingly high mortality rate. Azole-resistant Aspergillosis was found to kill 88% of patients who were infected. As the PLOS Pathogens study cited earlier describes:
In fact 50% of the patients with invasive aspergillosis due to ARAF are known to be azole na´ve and the outcome of patients with azole-resistant invasive aspergillosis has been dismal, with a mortality rate of 88%. (Van der Linden JWM, Snelders E, Kampinga GA, Rijnders BJA, Mattsson E, et al. (2011) Clinical implications of azole resistance in Aspergillus fumigatus, the Netherlands, 2007–2009. Emerg Infect Dis 17: 1846–1852.)
Even more alarmingly, it looks like patients currently being diagnosed as having chronic pulmonary infections may actually be victims of azole-resistant fungal infections. As the study explains, the genetic analysis (via PCR) of tissues from patients suffering chronic lung infections found that over half showed mutations characteristic of azole-resistant fungal strains:
[T]he same mechanism has also been reported in patients with chronic and allergic pulmonary infections [20]. For example, Denning et al. detected TR34/L98H and M220 mutations in 55.1% respiratory samples of CPA and ABPA patients by direct PCR…
This same genotype was, “found in 90% of ARAF isolates obtained from azole-na´ve patients,” the study reports, meaning it’s a near-certain sign that these patients have been colonized by azole-resistant fungal strains.
Chemical agriculture has unleashed a deadly global pathogen with no known medical treatment… and the entire medical establishment is burying the truth while exposing millions of hospital patients every day
The upshot of all this is that chemical agriculture has given rise to a deadly global pathogen that has spread across the globe and has no known medical treatment. The NYT article quotes Dr. Lynn Sosa, the deputy state epidemiologist for Connecticut, saying, “It’s pretty much unbeatable and difficult to identity.” That story adds that nearly 50% of patients who contract Candida auris are dead within 90 days, according to what appears to be reluctant statements from the CDC. There, the head of the fungal research branch, Dr. Tom Chiller, described the fungal superbug as “a creature from the black lagoon,” the NYT reported. “It bubbled up and now it is everywhere.”
Except that it didn’t have to be that way. There has been a cover-up for years. The very medical establishment that is entrusted with keeping people safe from deadly pathogens has, itself, become both the distribution hub for spreading the disease while simultaneously colluding with the CDC to hide the truth about all this from the public. It is the hospitals that are now “fungal factories” which are spreading the disease, literally releasing superbug pathogens into the open air, contaminating entire communities with fungal spores that are stronger than any treatment chemical known to western medicine.
There simply is no treatment, no cure, and very little honesty about the reality of the situation. To his credit, the CDC’s Dr. Chiller did post a warning about all this in 2017, but the CDC itself has refused to name the hospitals where these outbreaks are taking place.
The NYT describes the bizarre combination of panic and collusion that’s now taking place in hospitals across the world:
In late 2015, Dr. Johanna Rhodes, an infectious disease expert at Imperial College London, got a panicked call from the Royal Brompton Hospital, a British medical center outside London. C. auris had taken root there months earlier, and the hospital couldn’t clear it.
“‘We have no idea where it’s coming from. We’ve never heard of it. It’s just spread like wildfire,’” Dr. Rhodes said she was told. She agreed to help the hospital identify the fungus’s genetic profile and clean it from rooms.
Under her direction, hospital workers used a special device to spray aerosolized hydrogen peroxide around a room used for a patient with C. auris, the theory being that the vapor would scour each nook and cranny. They left the device going for a week. Then they put a “settle plate” in the middle of the room with a gel at the bottom that would serve as a place for any surviving microbes to grow, Dr. Rhodes said.
Only one organism grew back. C. auris.
It was spreading, but word of it was not. The hospital, a specialty lung and heart center that draws wealthy patients from the Middle East and around Europe, alerted the British government and told infected patients, but made no public announcement.
“There was no need to put out a news release during the outbreak,” said Oliver Wilkinson, a spokesman for the hospital.
This hushed panic is playing out in hospitals around the world. Individual institutions and national, state and local governments have been reluctant to publicize outbreaks of resistant infections, arguing there is no point in scaring patients — or prospective ones.
-
 Posting Permissions
Posting Permissions
- You may not post new threads
- You may not post replies
- You may not post attachments
- You may not edit your posts
-
Forum Rules

![[Most Recent Quotes from www.kitco.com]](http://www.kitconet.com/images/sp_en_6.gif)



 Reply With Quote
Reply With Quote